- Home
- Journal Contents Downloads
- JRSBRT Downloads
- JRSBRT 8.4, p. 247-255
Product Description
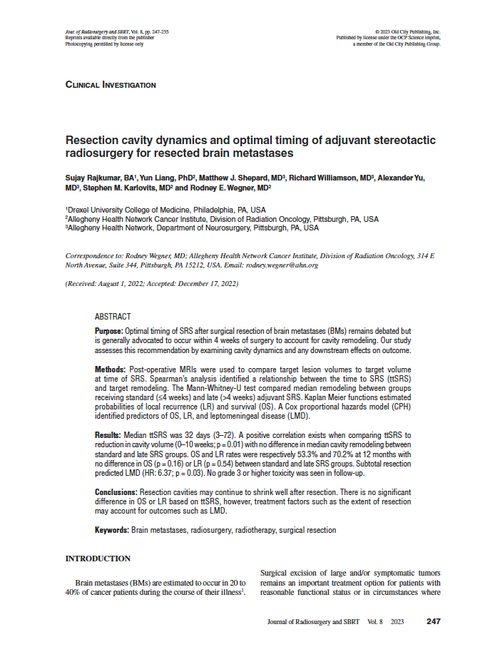
Resection cavity dynamics and optimal timing of adjuvant stereotactic radiosurgery for resected brain metastases
Sujay Rajkumar, Yun Liang, Matthew J. Shepard, Richard Williamson, Alexander Yu, Stephen M. Karlovits and Rodney E. Wegner
Purpose: Optimal timing of SRS after surgical resection of brain metastases (BMs) remains debated but is generally advocated to occur within 4 weeks of surgery to account for cavity remodeling. Our study assesses this recommendation by examining cavity dynamics and any downstream effects on outcome.
Methods: Post-operative MRIs were used to compare target lesion volumes to target volume at time of SRS. Spearman’s analysis identified a relationship between the time to SRS (ttSRS) and target remodeling. The Mann-Whitney-U test compared median remodeling between groups receiving standard (≤4 weeks) and late (>4 weeks) adjuvant SRS. Kaplan Meier functions estimated probabilities of local recurrence (LR) and survival (OS). A Cox proportional hazards model (CPH) identified predictors of OS, LR, and leptomeningeal disease (LMD).
Results: Median ttSRS was 32 days (3–72). A positive correlation exists when comparing ttSRS to reduction in cavity volume (0–10 weeks; p = 0.01) with no difference in median cavity remodeling between standard and late SRS groups. OS and LR rates were respectively 53.3% and 70.2% at 12 months with no difference in OS (p = 0.16) or LR (p = 0.54) between standard and late SRS groups. Subtotal resection predicted LMD (HR: 6.37; p = 0.03). No grade 3 or higher toxicity was seen in follow-up.
Conclusions: Resection cavities may continue to shrink well after resection. There is no significant difference in OS or LR based on ttSRS, however, treatment factors such as the extent of resection may account for outcomes such as LMD.
Keywords: Brain metastases, radiosurgery, radiotherapy, surgical resection
 Loading... Please wait...
Loading... Please wait...