- Home
- Journal Contents Downloads
- JRSBRT Downloads
- JRSBRT 5.2, p. 99-97
Product Description
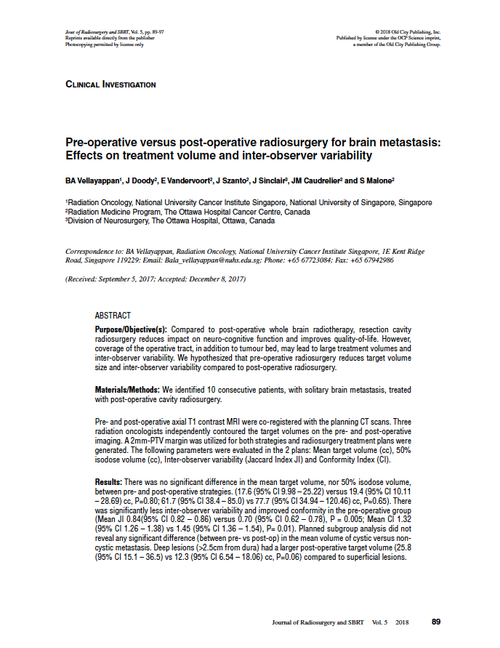
Pre-operative versus post-operative radiosurgery for brain metastasis: Effects on treatment volume and inter-observer variability
B.A. Vellayappan, J. Doody, E. Vandervoort, J. Szanto, J. Sinclair, J.M. Caudrelier and S. Malone
Purpose/Objective(s): Compared to post-operative whole brain radiotherapy, resection cavity radiosurgery reduces impact on neuro-cognitive function and improves quality-of-life. However, coverage of the operative tract, in addition to tumour bed, may lead to large treatment volumes and inter-observer variability. We hypothesized that pre-operative radiosurgery reduces target volume size and inter-observer variability compared to post-operative radiosurgery.
Materials/Methods: We identified 10 consecutive patients, with solitary brain metastasis, treated with post-operative cavity radiosurgery.
Pre- and post-operative axial T1 contrast MRI were co-registered with the planning CT scans. Three radiation oncologists independently contoured the target volumes on the pre- and post-operative imaging. A 2mm-PTV margin was utilized for both strategies and radiosurgery treatment plans were generated. The following parameters were evaluated in the 2 plans: Mean target volume (cc), 50% isodose volume (cc), Inter-observer variability (Jaccard Index JI) and Conformity Index (CI).
Results: There was no significant difference in the mean target volume, nor 50% isodose volume, between pre- and post-operative strategies. (17.6 (95% CI 9.98 – 25.22) versus 19.4 (95% CI 10.11 – 28.69) cc, P=0.80; 61.7 (95% CI 38.4 – 85.0) vs 77.7 (95% CI 34.94 – 120.46) cc, P=0.65). There was significantly less inter-observer variability and improved conformity in the pre-operative group (Mean JI 0.84(95% CI 0.82 – 0.86) versus 0.70 (95% CI 0.62 – 0.78), P = 0.005; Mean CI 1.32 (95% CI 1.26 – 1.38) vs 1.45 (95% CI 1.36 – 1.54), P= 0.01). Planned subgroup analysis did not reveal any significant difference (between pre- vs post-op) in the mean volume of cystic versus noncystic metastasis. Deep lesions (>2.5cm from dura) had a larger post-operative target volume (25.8 (95% CI 15.1 – 36.5) vs 12.3 (95% CI 6.54 – 18.06) cc, P=0.06) compared to superficial lesions.
Conclusion: Pre-operative radiosurgery has less inter-observer variability and improved plan conformity. However, there was no difference in mean target volume between the pre- versus postoperative radiation. Contouring guidelines, and peer review, may help to reduce inter-observer variability for cavity radiosurgery.
Keywords: brain metastasis, radiosurgery, adjuvant, pre-operative
After payment has been processed for your order of a digital copy (PDF) of this article, you will see a download link on your completed order page and also receive an email containing a download link. The links, which will enable you to download one copy of the article, will expire after 24 hours.
 Loading... Please wait...
Loading... Please wait...